Ear Injuries in Diving
by Michael RothschildOriginally published in Adventure Diving Magazine, December/January 2013
Cover photo by Michael Rothschild
INTRODUCTION
As a medical moderator for an online scuba forum, I answer more questions about dive related ear problems than anything else. The ear is uniquely positioned to be vulnerable to both external and internal injury when diving. Furthermore, there is a great deal of confusion about the nature of these problems - the relevant anatomy, the causes of symptoms and the best treatment.
To make things worse, even people who have obtained medical care may have no better understanding of the source of their pain, dizziness or hearing loss. This is because even for many brilliant and experienced general physicians, the ear can be very difficult to examine. I realize that this sounds arrogant on my part - believe me, I am humble about my own skills and deferential to GPs who must be able to manage a wide range of life threatening conditions. However, the fact remains that many doctors who are not otolaryngologists (ENTs) do not have the specialized equipment or experience necessary to clean the ear thoroughly, to examine the eardrum under high magnification, and to test hearing in a comprehensive manner.
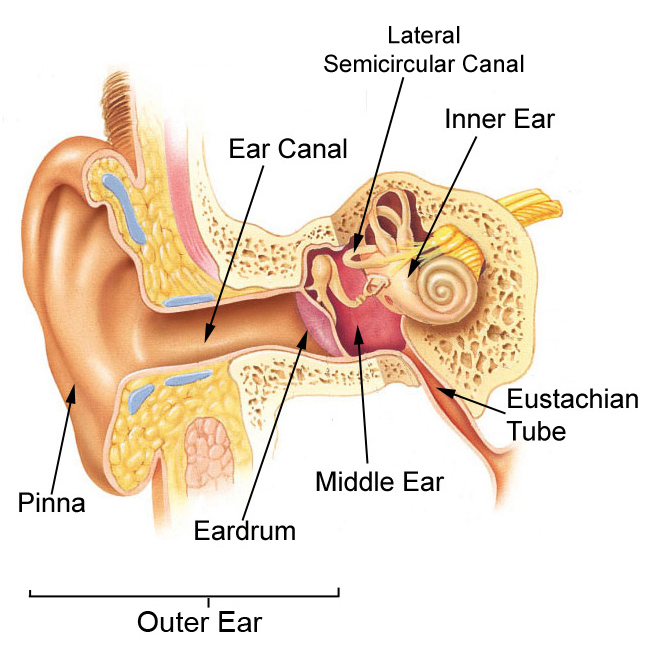
One of the greatest sources of confusion is the fact that the outer ear, middle ear and inner ear - which are completely different systems that have very little to do with each other - often can give rise to similar symptoms such as ear pain, vertigo or hearing problems. So let's review each of the three main parts of the ear, and see how diving can affect them.
OUTER EAR
The outer ear refers to the part that sticks out of the head (the pinna) and the hole that leads to a tube (the ear canal) that ends at the eardrum. It is basically a pocket of skin, and it is where earwax (cerumen) is created and accumulates. Cerumen is a normal substance which protects the ear canal - it is generally just a thin layer coating the walls, but some people accumulate large amounts of it. It consists mostly of dead skin, mixed with various oily secretions from glands in the outer ear.
When water gets into the ear from swimming or diving, it gets into the ear canal. This is an important concept - unless there is a hole in the eardrum, the water from swimming or diving does not enter the middle ear.
Water from swimming or diving can get stuck in the external ear canal, especially if there is a lot of earwax. Furthermore, wet earwax takes a long time to dry out. Just like in cases of diaper rash or athlete’s foot, when an area of the body is kept damp and dirty, it leads to chronic inflammation and swelling, with skin breakdown and infection (usually with the pseudomonas bacteria that normally lives in this area). This inflammatory condition of the outer ear is called “swimmer’s ear” or otitis externa, and it can be extremely painful.
People who spend a lot of time in cold water can get bony growths in their ear canals (osteomas, or "surfer's ear"). These can trap earwax and water if they get big enough. The growths occasionally require surgical removal.
Treatment of swimmer’s ear is helped by carefully cleaning the wet debris from the ear canal to allow the ear to dry. This is best done by an ENT doctor using a microscope and small ear tools, under direct vision. This will also allow for a high magnification inspection of the eardrum, to rule out a perforation or other middle ear problems. Once the ear is clean, medicated ear drops are used, generally those containing an antibiotic to kill the bacteria, and a steroid to help with the swelling and pain.
A number of things can be done to prevent swimmer’s ear. Disimpaction of large accumulations of wax (under direct vision, ideally with a microscope) will help avoid water trapping. But overly aggressive and frequent ear cleaning can actually make the situation worse, by removing the protective layer of cerumen. Drying the ear after swimming can help as well. A good way to do this is with a dedicated ear dryer, which blows a gentle stream of warm air into the ear canal.
Another approach to prevention of swimmer’s ear is the use of 5-10 drops of a solution of rubbing alcohol and white vinegar after diving. Add three tablespoons of the vinegar to a pint of the alcohol. Unlike the 50-50 mixes which are sometimes recommended, this makes a mixture that does not have a lot of water in it. The alcohol dries the ear, and the vinegar makes the ear canal more acidic, which makes it harder for the pseudomonas bacteria to grow. Avoid overuse of this solution, as it can overdry the ear, breaking down the protective layer of earwax and causing irritation - no more than once or twice a day. A few drops of glycerine in the mix can help prevent overdrying. Cotton tipped applicators should never be used - they tend to pack the wax into the ear canal, and can cause permanent injury if they touch the eardrum.
MIDDLE EAR
The middle ear is the space behind the eardrum. It is lined with mucosa, which is the same sort of "skin" that lines the mouth and nose. It also contains the three bones of hearing, which carry sound vibrations from the eardrum to the inner ear (see below). The middle ear is basically an extension of the upper airway, and is connected to the back of the nose by a tunnel called the Eustachian tube (ET). The walls of this tunnel are supported by cartilage, which tends to spring back into the normally closed position after being forced open (either by muscle action or by pressure changes in the airway from diving or from ear clearing maneuvers).
Diving injuries to the middle ear are the result of barotrauma, which is damage caused by pressure changes. As every certified diver knows, diving requires equalization of the pressure outside of the body with that inside, otherwise a big pressure gradient occurs causing pain and eventually damage. Since fluid is essentially not compressible, there are only significant pressure gradients in the air filled spaces of the body.
Most of the air in the body is in the airways - the lungs, the windpipe, the larynx (voicebox), the throat, mouth and nose. All of these spaces are connected by wide passages, so pressure changes occur everywhere at once in the airway, as a regulator delivers gas at ambient pressure (proportional to depth).
There is also a small amount of air in other spaces in the body - the middle ears, the nasal sinuses, and sometimes the teeth (especially underneath dental work). These spaces are connected to the airways as well, but by small passages that may be blocked at times. Therefore, it is possible to build up a big pressure gradient in these spaces during descent, if a diver is not careful to equalize fully.
To equalize the ears, the diver must allow the ET to open against a pressure gradient. This can be done by a number of maneuvers taught in basic open water scuba instruction. Pinching the nose and blowing (Valsalva maneuver) and pinching and swallowing (Toynbee maneuver) are common methods for equalization, but many divers learn to open a blocked ET by other approaches, such as moving the jaw, tensing the roof of the mouth, etc...
A failure to equalize on descent can result in a block - a situation when the pressure gradient itself makes it harder for the ET to open, which results in a further gradient if descent is continued, leading to a “vicious cycle”. The solution here is to stop the descent (or ascend a bit if necessary) until equalization is possible. A less common situation is a reverse block, which happens on ascent. The reason this is less common is that with a poorly functioning ET, the change in middle ear gas pressure with ascent or descent lags the change in ambient pressure. Therefore, with ascent you have higher pressure in the middle ear than in the airway. This pressure gradient tends to overcome a blocked ET - the air “forces” it’s way out. It’s something like the fact that it is easier to squeeze toothpaste out of a tube than to put it back in.
A prolonged or significant pressure gradient in the middle ear can result in some type of barotrauma. This can be a perforated eardrum (the eardrum acts like the burst disk in the scuba tank, and gives way when subjected to enough pressure). If the eardrum doesn’t perforate, fluid with or without blood can accumulate in the middle ear space. Unlike the middle ear infections that young children get, this fluid is clean with no bacteria. Clear fluid is called an “effusion”, and a bloody effusion is called a “hemotympanum”. The effusion is actually the result of fluid in the bloodstream (plasma) filtering into the middle ear when following the pressure gradient.
Fluid in the middle ear causes a temporary hearing loss by preventing the normal vibration of the eardrum with sound. It is a “conductive” hearing loss - the problem is that the mechanism that conducts sound into the inner ear is not working well. There is nothing wrong in this case with the sensory organ (the cochlea) or the nerves to the brain - if there were, it would result in a (usually permanent) “sensorineural” hearing loss, which we will discuss in the next section.
Some people have more trouble with this than others, due to dysfunction of the Eustachian tube (ETD). Many divers always need a long time to descend and ascend since their ETs don’t work very well at baseline. Other people may have no problem equalizing in general, but find it more difficult when a cold or other infection causes congestion of the lining of the ET. This is often oversimplified as the ET being "small" or "narrow" - the true problem is more of a functional issue with the structure of the tube istelf (for example, with the muscles that normally open the tube). Another common misconception is that fixing nasal obstruction, for example by straightening a deviated nasal septum, will help the function of the ET. While there is some overlap between overall nasal blockage and ET function as mentioned above, most of the areas of the nose which require treatment to improve breathing are nowhere near the ET opening.
A single eardrum perforation related to barotrauma (without a history of ear disease) usually heals by itself over weeks to months, but no diving is allowed until the eardrum is once again intact. In some cases, surgery will be needed to seal the hole in the drum. Middle ear effusion typically resolves over time, and can be helped to resolve by the same sort of ET opening maneuvers described above. Antibiotics are generally not necessary.
Many divers swear by the use of decongestants and/or nasal steroid sprays to treat this problem or prevent its development. While these drugs can help prevent barotrauma of the nasal sinuses, there is not much data to suggest that they help middle ear disease any more than time and the ET maneuvers alone. Oral steroids can help the ears drain an effusion, but these drugs have many side effects and are rarely used in this situation. Motrin and other non-steroidal anti-inflammatory drugs may help with the pain, but have little effect on ET function. In some cases (when no more diving is planned for a long time) an ENT doctor can make a small hole in the eardrum to drain the effusion if it is causing severe symptoms (hearing loss, a blocked sensation in the ear, or dizziness).
There is not a lot that can be done directly to treat a poorly functioning ET. If the ETD is caused by a temporary problem (like a cold or other infection), then ear ventilation usually returns to baseline when the airway congestion resolves. Divers with longstanding baseline ETD usually address the problem by finding a maneuver that works to allow them to equalize. Although there are some experimental treatments involving procedures to stretch the ET open, there isn't a lot of data at this point about the risks and benefits of such operations.
INNER EAR
The inner ear is deep inside the skull, and is an extension of the brain. It contains the cochlea, which is the organ of hearing (like the retina in the eye) that converts sound vibrations into electrical impulses that the brain can interpret as sound. It also contains the labyrinth, which is the organ of balance. The inner ear is behind a bony wall at the back of the middle ear, and connects with the middle ear through two small holes in the bone, which are normally sealed to prevent leakage of fluid or gas. Unlike outer and middle ear problems, inner ear injuries cannot be seen by looking into the ear canal.
Diving related inner ear problems are very rare, but have the potential to cause permanent hearing loss. There are two types that can result in serious injury- inner ear decompression sickness (IEDCS) and inner ear barotrauma. These require immediate attention, and in the case of barotrauma, emergency surgery may be necessary.
A thorough discussion of IEDCS is beyond the scope of this article, and the exact mechanism of this condition is still unclear. However, every certified diver has learned about the risk of bubble formation in the tissues with ascent, especially when inert gas (e.g. nitrogen) loading is high. Like other forms of decompression illness, IEDCS results in hearing loss or vertigo (a sensation of the world spinning around) due to bubble formation. It is not known for sure whether the bubbles form in the inner ear fluid directly, or form in the veins of the bloodstream and are carried to the inner ear through abnormal connections between the veins and the arteries (e.g. a patent foramen ovale or other shunts in the lung circulation).
Inner ear barotrauma can happen in two ways, but they both involve a sudden pressure change in the inner ear fluid (known as perilymph). A rapid increase in middle ear pressure happens when a blocked ET suddenly opens during equalization. This can cause the stapes (the bone that connects the middle and inner ear spaces) to pull sharply out of its normal position, resulting in the inner ear fluid being sucked inward, breaking the seal at the round window. Also, a forceful Valsalva maneuver can cause an increase in inner ear pressure, pushing the round window membrane outwards, into the middle ear. The resulting “perilymph fistula” (PLF) with leakage of inner ear fluid can cause nausea, vertigo, and a progressive and often permanent sensorineural hearing loss.
Diagnosis of inner ear problems can be difficult, as the eardrum looks normal on exam. DCS may be suggested by the dive profile and other associated symptoms, and rapid treatment with oxygen, hydration and recompression in a hyperbaric chamber are essential. However, recompression may make inner ear barotrauma worse, so careful evaluation by a specialist in this area is crucial.
A formal hearing test can distinguish between conductive and sensorineural hearing loss, and therefore should be a part of the evaluation of any diving related ear injury. Other tests include an assessment of the function of the balance mechanism, which can be measured in a special lab. A CT scan is rarely helpful, as a PLF cannot be seen on an x-ray.
When there is enough of a suspicion of a PLF, an operation is usually recommended; this condition can only be definitively diagnosed by surgical exploration of the ear. The procedure involves lifting up the eardrum to visualize the middle ear directly. If what looks like inner ear fluid is seen leaking from the space around the round window (or anywhere else), fat grafts are used to seal the area. This leakage can be very subtle, as the volume of perilymph is small. However, early closure of a PLF can mean the difference between a recovery of hearing and a progression to complete deafness. Since the operation itself involves very little risk, it should be strongly considered in cases where PLF is a possibility.
There are two other ways that the inner ear can be abnormally stimulated during a dive, causing dizziness - cold caloric responses and altenobaric vertigo (ABV). Both of these are due to the balance portions of the left and right inner ears being stimulated to different degrees. When the nerve from one inner ear has more activity than the other, the brain gets "confusing" inputs - normally both inner ears send the same information when the body moves in three dimensional space. The brain's response to this assymetric input is vertigo.
The caloric phenomenon is the result of a sudden temperature change in one of the diver's inner ears. The semicircular canals are a part of the balance mechanism in the inner ear, and one of them (the lateral canal) is near the eardrum. Cold water entering one of the outer ear canals can result in motion in the fluid inside that lateral canal as the cooled fluid sinks. This results in activity in the nerve to the brain from that inner ear. ABV is due to assymmetric equalization during the dive, where the middle ear pressure (transmitted to the inner ear) is greater on one side than the other.
Both of these conditions are generally temporary, and resolve as the temperature stabilizes and the flow stops, or as equalization is completed in both ears, but it can be very disconcerting to have sudden dizziness during a dive. Awareness of this phenomenon and taking any steps necessary to address it (such as careful and thorough equalization) can prevent a spiral into panic and bad decisions.
CONCLUSION
The vast majority of ear pain after diving goes away by itself in a short time. However, without an examination, a diver may not be able to tell whether the problem is in the outer or middle ear, and treatment depends on accurate diagnosis. Hearing loss after diving should be evaluated soon, and by formal testing. Thorough evaluation of persistent ear problems should be done by a doctor with the tools and experience necessary to distinguish outer, middle and inner ear disease.